Important information on dental health everyone should read concerning Dr. Weston Price’s research, what root canals do to our health, and what a root canal is. They are not the only option available to people. May this information be a blessing to you and I ask our Well Beloved FATHER in Heaven for whatever help you need for now and for eternity in the Precious NAME of HIS Beloved SON, JESUS CHRIST the LORD/YAHSHUA HA’MASHIACH YHWH, AMEN!
http://articles.mercola.com/sites/articles/archive/2010/11/16/why-you-should-avoid-root-canals-like-the-plague.aspx
Why You Should Avoid Root Canals Like the Plague
Many people have had questions about root canals, so I thought it would be wise to repost this article.
It was an interview with Dr. George Meinig, who was dentist and leader in teaching people about the dangers of root canals. He wrote the book Root Canal Cover Up.
Because I first became aware of this information in the early ’90s I was able to avoid having any root canals. I elected to have three teeth extracted and now have two bridges to replace those teeth.
At the time, that was my best option, as I believe that metal implants should be avoided. However in the last few years non-reactive metal implants made from zirconium have become available and that is what I would use now if I had to have an alternative to a root canal.
Why I Encourage You to Think Twice Before Getting a Root Canal
Please don’t let your dentist mislead you that a root canal is your only option, or that it is entirely safe.
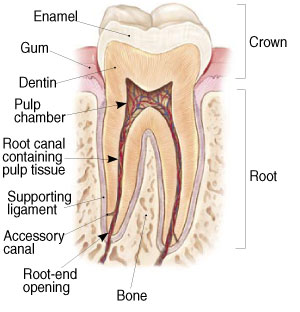
Teeth are similar to other organ systems in your body in that they also require a blood supply, lymphatic, and venous drainage, and nervous innervations. Root canals, however, are dead teeth, and these dead teeth typically become one of, if not the worst, sources of chronic bacterial toxicity in your body.
If your kidney, liver, or any other organ in your body dies, it will have to be removed so that bacteria and necrosis will not set in and kill you… but teeth are commonly left dead in your body.
Teeth have roots with main canals and thousands of side canals, and contained in those side canals are miles of nerves. When dentists perform a root canal, they remove the nerve from the main canals; however they do not have access to the microscopic side canals, which have dead nerves left behind in those spaces.
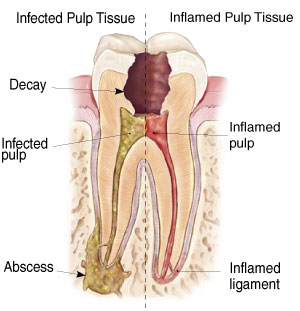
Anaerobic bacteria, which do not require oxygen to survive, thrive in these side canals and excrete toxicity from digesting necrotic tissue that leads to chronic infection. Blood supply and lymphatics that surround those dead teeth drains this toxicity and allows it to spread throughout your body. This toxicity will invade all organ systems and can lead to a plethora of diseases such as autoimmune diseases, cancers, musculoskeletal diseases, irritable bowel diseases, and depression, to name just a few.
Even antibiotics won’t help in these cases, because the bacteria are protected inside of your dead tooth.
It appears that the longer root canal-treated teeth stay in your body, the more your immune system becomes compromised.
Seek Out a Biological Dentist Who Is Aware of Root Canal Dangers
If your dentist is not actively engaged in continuing education, and is not open to alternative, toxin-free forms of dentistry, there’s a good chance he or she is not aware of the risks of — and alternatives to — root canals. A biological dentist will be able to provide you with a more comprehensive, holistic solution for your teeth that will not harm your health.
Knowledgeable biological dentists can be hard to come by, so start your search by asking a friend, relative, or neighbor who knows of one. If that fails you can contact several good natural health food stores in your area and ask a number of the employees or even the owner. The following links can also help you to find a biological dentist:
- Dental Amalgam Mercury Solutions: e-mail [email protected] or call for an information packet
- Consumers for Dental Choice
- International Academy of Biological Dentistry and Medicine
- International Academy of Oral Medicine and Toxicology
- Holistic Dental Association
- International Association of Mercury Safe Dentists
An Interview with George Meinig, D.D.S.
Dr. Meinig brings an interesting perspective to expose the latent dangers of root canal therapy. Dr. Meinig is particularly well qualified to comment on this topic as 60 years ago he was one of the founders of the American Association of Endodontists (root canal specialists)!
So he’s filled his share of root canals — and when he wasn’t filling canals himself, he was teaching the technique to dentists across the country at weekend seminars and clinics.
After he retired he decided to read all 1,174 pages of the detailed research of Dr. Weston Price, (D.D.S.). Dr. Meinig was startled and shocked as he found a valid documentation of systemic illnesses resulting from latent infections lingering in filled roots.
After reviewing Dr. Price’s materials he wrote Root Canal Cover Up.
Please explain what the problem is with root canal therapy.
GM: First, let me note that my book is based on Dr. Weston Price’s 25 years of careful, impeccable research. He led a 60-man team of researchers whose findings — suppressed until now rank right up there with the greatest medical discoveries of all time. This is not the usual medical story of a prolonged search for the difficult-to-find causative agent of some devastating disease.
Rather, it’s the story of how a “cast of millions” (of bacteria) become entrenched inside the structure of teeth and end up causing the largest number of diseases ever traced to a single source.
What diseases? Can you give us some examples?
GM: Yes, a high percentage of chronic degenerative diseases can originate from root filled teeth. The most frequent were heart and circulatory diseases and he found 16 different causative agents for these.
The next most common diseases were those of the joints, arthritis and rheumatism. In third place — but almost tied for second — were diseases of the brain and nervous system. After that, any disease you can name might (and in some cases has) come from root filled teeth.
Let me tell you about the research itself. Dr. Price undertook his investigations in 1900. He continued until 1925, and published his work in two volumes in 1923. In 1915 the National Dental Association (which changed its name a few years later to The American Dental Association) was so impressed with his work that they appointed Dr. Price their first Research Director.\
His Advisory Board read like a Who’s Who in medicine and dentistry for that era. They represented the fields of bacteriology, pathology, rheumatology, surgery, chemistry, and cardiology.
At one point in his writings Dr. Price made this observation: “Dr. Frank Billings (M.D.), probably more than any other American internist, is due credit for the early recognition of the importance of streptococcal focal infections in systemic involvements.”
What’s really unfortunate here is that very valuable information was covered up and totally buried some 70 years ago by a minority group of autocratic doctors who just didn’t believe or couldn’t grasp – the focal infection theory.
What is the “focal infection” theory?
GM: This states that germs from a central focal infection — such as your teeth, teeth roots, inflamed gum tissues, or maybe tonsils — metastasize to hearts, eyes, lungs, kidneys, or other organs, glands and tissues, establishing new areas of the same infection.
Hardly theory any more, this has been proven and demonstrated many times over. It’s 100 percent accepted today. But it was revolutionary thinking during World War I days, and the early 1920’s!
Today, both patients and physicians have been “brainwashed” to think that infections are less serious because we now have antibiotics. Well, yes and no. In the case of root-filled teeth, the no longer-living tooth lacks a blood supply to its interior. So circulating antibiotics don’t faze the bacteria living there because they can’t get at them.
You’re assuming that ALL root-filled teeth harbor bacteria and/or other infective agents?
GM: Yes. No matter what material or technique is used — and this is just as true today — the root filling shrinks minutely, perhaps microscopically. Further and this is key — the bulk of solid appearing teeth, called the dentin, actually consists of miles of tiny tubules.
Microscopic organisms lurking in the maze of tubules simply migrate into the interior of the tooth and set up housekeeping. A filled root seems to be a favorite spot to start a new colony.
One of the things that makes this difficult to understand is that large, relatively harmless bacteria common to the mouth change and adapt to new conditions. They shrink in size to fit the cramped quarters and even learn how to exist (and thrive!) on very little food. Those that need oxygen mutate and become able to get along without it.
In the process of adaptation these formerly friendly “normal” organisms become pathogenic (capable of producing disease) and more virulent (stronger) and they produce much more potent toxins.
Today’s bacteriologists are confirming the discoveries of the Price team of bacteriologists. Both isolated in root canals the same strains of streptococcus, staphylococcus, and spirochetes.
Is everyone who has ever had a root canal filled made ill by it?
GM: No. We believe now that every root canal filling does leak and bacteria do invade the structure. But the variable factor is the strength of the person’s immune system.
Some healthy people are able to control the germs that escape from their teeth into other areas of the body. We think this happens because their immune system lymphocytes (white blood cells) and other disease fighters aren’t constantly compromised by other ailments. In other words, they are able to prevent those new colonies from taking hold in other tissues throughout the body.
But over time, most people with root filled teeth do seem to develop some kinds of systemic symptoms they didn’t have before.
It’s really difficult to grasp that bacteria are embedded deep in the structure of seemingly hard, solid-looking teeth.
GM: I know. Physicians and dentists have that same problem, too. You really have to visualize the tooth structure — all of those microscopic tubules running through the dentin. In a healthy tooth, those tubules transport a fluid that carries nourishment to the inside. For perspective, if the tubules of a front single-root tooth were stretched out on the ground they’d stretch for three miles!
A root filled tooth no longer has any fluid circulating through it, but the maze of tubules remains. The anaerobic bacteria that live there seem remarkably safe from antibiotics. The bacteria can migrate out into surrounding tissue where they can “hitchhike” to other locations in the body via the bloodstream.
The new location can be any organ or gland or tissue, and the new colony will be the next focus of infection in a body plagued by recurrent or chronic infections.
All of the “building up” done to try to enhance the patient’s ability to fight infections – to strengthen their immune system – is only a holding action. Many patients won’t be well until the source of infection – the root canal tooth – is removed.
I don’t doubt what you’re saying, but can you tell us more about how Dr. Price could be sure that arthritis or other systemic conditions and illnesses really originated in the teeth — or in a single tooth?
GM: Yes. Many investigations start with the researcher just being curious about something – and then being scientifically careful enough to discover an answer, and then prove it’s so, many times over.
Dr. Price’s first case is very well documented. He removed an infected tooth from a woman who suffered from severe arthritis.
As soon as he finished with the patient, he implanted the tooth beneath the skin of a healthy rabbit. Within 48 hours the rabbit was crippled with arthritis!
Further, once the tooth was removed the patient’s arthritis improved dramatically. This clearly suggested that the presence of the infected tooth was a causative agent for both that patient’s and the rabbit’s – arthritis.
Here’s the actual story of that first patient from Dr. Meinig’s book:
“(Dr. Price) had a sense that, even when (root canal therapy) appeared successful, teeth containing root fillings remained infected. That thought kept prying on his mind, haunting him each time a patient consulted him for relief from some severe debilitating disease for which the medical profession could find no answer.
Then one day while treating a woman who had been confined to a wheelchair for six years from severe arthritis, he recalled how bacterial cultures were taken from patients who were ill and then inoculated into animals in an effort to reproduce the disease and test the effectiveness of drugs on the disease.
With this thought in mind, although her (root filled) tooth looked fine, he advised this arthritic patient, to have it extracted. He told her he was going to find out what it was about this root filled tooth that was responsible for her suffering.
“All dentists know that sometimes arthritis and other illnesses clear up if bad teeth are extracted. However, in this case, all of her teeth appeared in satisfactory condition and the one containing this root canal filling showed no evidence or symptoms of infection. Besides, it looked normal on x-ray pictures.
“Immediately after Dr. Price extracted the tooth he dismissed the patient and embedded her tooth under the skin of a rabbit. In two days the rabbit developed the same kind of crippling arthritis as the patient – and in ten days it died.
“..The patient made a successful recovery after the tooth’s removal! She could then walk without a cane and could even do fine needlework again. That success led Dr. Price to advise other patients, afflicted with a wide variety of treatment defying illnesses, to have any root filled teeth out.”
In the years that followed, he repeated this procedure many hundreds of times. He later implanted only a portion of the tooth to see if that produced the same results. It did. He then dried the tooth, ground it into powder and injected a tiny bit into several rabbits. Same results, this time producing the same symptoms in multiple animals.
Dr. Price eventually grew cultures of the bacteria and injected them into the animals. Then he went a step further. He put the solution containing the bacteria through a filter small enough to catch the bacteria. So when he injected the resulting liquid it was free of any infecting bacteria. Did the test animals develop the illness? Yes.
The only explanation was that the liquid had to contain toxins from the bacteria, and the toxins were also capable of causing disease.
Dr. Price became curious about which was the more potent infective agent, the bacteria or the toxin. He repeated that last experiment, injecting half the animals with the toxin-containing liquid and half of them with the bacteria from the filter. Both groups became ill, but the group injected with the toxins got sicker and died sooner than the bacteria injected animals.”]
That’s amazing. Did the rabbits always develop the same disease the patient had?
GM: Mostly, yes. If the patient had heart disease the rabbit got heart disease. If the patient had kidney disease the rabbit got kidney disease, and so on. Only occasionally did a rabbit develop a different disease — and then the pathology would be quite similar, in a different location.
If extraction proves necessary for anyone reading this, do you want to summarize what’s special about the extraction technique?
GM: Just pulling the tooth is not enough when removal proves necessary. Dr. Price found bacteria in the tissues and bone just adjacent to the tooth’s root. So we now recommend slow-speed drilling with a burr, to remove one millimeter of the entire bony socket.
The purpose is to remove the periodontal ligament (which is always infected with toxins produced by streptococcus bacteria living in the dentin tubules) and the first millimeter of bone that lines the socket (which is usually infected).
There’s a whole protocol involved, including irrigating with sterile saline to assure removal of the contaminated bone chips, and treating the socket to stimulate and encourage infection-free healing. I describe the procedure in detail, step by step, in my book [pages 185 and 186].
Perhaps we should back up and talk about oral health — to PREVENT needing an extraction. Caries or inflamed gums seem much more common than root canals. Do they pose any threat?
GM: Yes, they absolutely do. But let me point out that we can’t talk about oral health apart from total health. The problem is that patients and dentists alike haven’t come around to seeing that dental caries reflect systemic — meaning “whole body” — illness.
Dentists have learned to restore teeth so expertly that both they and their patients have come to regard tooth decay as a trivial matter. It isn’t.
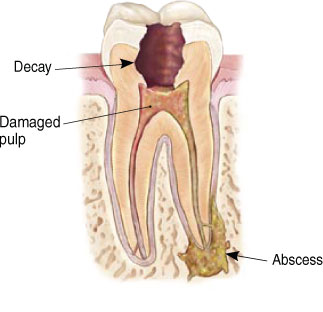
Small cavities too often become big cavities. Big cavities too often lead to further destruction and the eventual need for root canal treatment.
Then talk to us about prevention.
GM: The only scientific way to prevent tooth decay is through diet and nutrition. Dr. Ralph Steinman did some outstanding, landmark research at Loma Linda University. He injected a glucose solution into mice — into their bodies, so the glucose didn’t even touch their teeth. Then he observed the teeth for any changes. What he found was truly astonishing.
The glucose reversed the normal flow of fluid in the dentin tubules, resulting in all of the test animals developing severe tooth decay! Dr. Steinman demonstrated dramatically what I said a minute ago:
Dental caries reflect systemic illness.
Let’s take a closer look to see how this might happen. Once a tooth gets infected and the cavity gets into the nerve and blood vessels, bacteria find their way into those tiny tubules of the dentin. Then no matter what we do by way of treatment, we’re never going to completely eradicate the bacteria hiding in the miles of tubules.
In time the bacteria can migrate through lateral canals into the surrounding bony socket that supports the tooth. Now the host not only has a cavity in a tooth, plus an underlying infection of supporting tissue to deal with, but the bacteria also exude potent systemic toxins.
These toxins circulate throughout the body triggering activity by the immune system — and probably causing the host to feel less well.
This host response can vary from just dragging around and feeling less energetic, to overt illness — of almost any kind.
Certainly, such a person will be more vulnerable to whatever “bugs” are going around, because his/her body is already under constant challenge and the immune system continues to be “turned on” by either the infective agent or its toxins — or both.
What a fascinating concept. Can you tell us more about the protective nutrition you mentioned?
GM: Yes. Dr. Price traveled all over the world doing his research on primitive peoples who still lived in their native ways. He found 14 cultural pockets scattered all over the globe where the natives had no access to “civilization” – and ate no refined foods.
Dr. Price studied their diets carefully. He found they varied greatly, but the one thing they had in common was that they ate whole, unrefined foods. With absolutely no access to tooth brushes, floss, fluoridated water, or toothpaste, the primitive peoples studied were almost 100% free of tooth decay.
Further — and not unrelated — they were also almost 100% free of all the degenerative diseases we suffer — problems with the heart, lungs, kidneys, liver, joints, skin (allergies), and the whole gamut of illnesses that plague Mankind. No one food proved to be magic as a preventive food. I believe we can thrive best by eating a wide variety of whole foods.
Amazing. So by “diet and nutrition” for oral (and total) health you meant eating a pretty basic diet of whole foods?
GM: Exactly. And no sugar or white flour. These are (and always have been) the first culprits. Tragically, when the primitives were introduced to sugar and white flour their superior level of health deteriorated rapidly. This has been demonstrated time and again.
During the last 60 or more years we have added, in increasing amounts, highly refined and fabricated cereals and boxed mixes of all kinds, soft drinks, refined vegetable oils, and a whole host of other foodless “foods.”
It is also during those same years that we as a nation have installed more and more root canal fillings — and degenerative diseases have become rampant. I believe — and Dr. Price certainly proved to my satisfaction — that these simultaneous factors are NOT coincidences.
I certainly understand what you are saying. But I’m still a little shocked to talk with a dentist who doesn’t stress oral hygiene.
GM: Well, I’m not against oral hygiene. Of course, hygiene practices are preventive, and help minimize the destructive effect of our “civilized,” refined diet. But the real issue is still diet. The natives Dr. Price tracked down and studied weren’t free of cavities, inflamed gums, and degenerative diseases because they had better tooth brushes!
It’s so easy to lose sight of the significance of what Dr. Price discovered. We tend to sweep it under the rug — we’d actually prefer to hear that if we would just brush better, longer, or more often, we too could be free of dental problems.
Certainly, part of the purpose of my book is to stimulate dental research into finding a way to sterilize dentin tubules. Only then can dentists really learn to save teeth for a lifetime.
But the bottom line remains: A primitive diet of whole unrefined foods is the only thing that has been found to actually prevent both tooth decay and degenerative diseases.
For More Information
Dr. Meinig’s Root Canal Cover Up and Dr. Price’s book Nutrition and Physical Degeneration can be purchased at the Price Pottinger Foundation.
Below is information on understanding what a root canal is.
|
| Endodontic Procedure
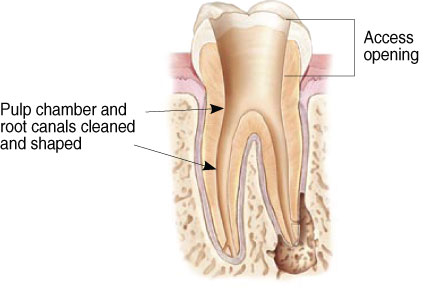
Endodontic treatment can often be performed in one or two visits and involves the following steps: 1. The endodontist examines and x-rays the tooth, then administers local anesthetic. After the tooth is numb, the endodontist places a small protective sheet called a ‘dental dam’over the area to isolate the tooth and keep it clean and free of saliva during the procedure.
|
| 2. The endodontist makes an opening in the crown of the tooth. Very small instruments are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling.
|
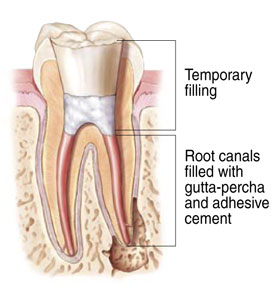
| 3. After the space is cleaned and shaped, the endodontist fills the root canals with a biocompatible material, usually a rubber-like material called ‘gutta-percha.’The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals. In most cases, a temporary filling is placed to close the opening. The temporary filling will be removed by your dentist before the tooth is restored.
|
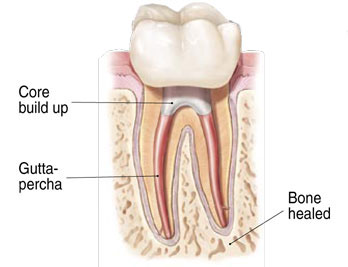
| 4. After the final visit with your endodontist, you must return to your dentist to have a crown or other restoration placed on the tooth to protect and restore it to full function.
|
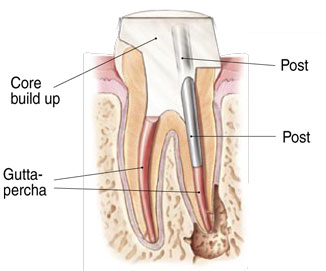
| If the tooth lacks sufficient structure to hold the restoration in place, your dentist or endodontist may place a post inside the tooth. Ask your dentist or endodontist for more details about the specific restoration planned for your tooth.
|
How much will the procedure cost?
The cost varies depending on how complex the problem is and which tooth is affected. Molars are more difficult to treat, the fee is usually more. Most dental insurance policies provide some coverage for endodontic treatment.
Generally, endodontic treatment and restoration of the natural tooth are less expensive than the alternative of having the tooth extracted. An extracted tooth must be replaced with a bridge or implant to restore chewing function and prevent adjacent teeth from shifting. These procedures tend to cost more than endodontic treatment and appropriate restoration. With root canal treatment you save your natural teeth and money.
Will the tooth need any special care or additional treatment after endodontic treatment?
You should not chew or bite on the treated tooth until you have had it restored by your dentist. The unrestored tooth is susceptible to fracture, so you should see your dentist for a full restoration as soon as possible. Otherwise, you need only practice good oral hygiene, including brushing, flossing, and regular checkups and cleanings.
Most endodontically treated teeth last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic treatment does not heal or the pain continues. Occasionally, the tooth may become painful or diseased months or even years after successful treatment. Often when this occurs, redoing the endodontic procedure can save the tooth.
What causes an endodontically treated tooth to need additional treatment?
New trauma, deep decay, or a loose, cracked or broken filling can cause new infection in your tooth. In some cases, the endodontist may discover additional very narrow or curved canals that could not be treated during the initial procedure.
Can all teeth be treated endodontically?
Most teeth can be treated. Occasionally, a tooth can’t be saved because the root canals are not accessible, the root is severely fractured, the tooth doesn’t have adequate bone support, or the tooth cannot be restored. However, advances in endodontics are making it possible to save teeth that even a few years ago would have been lost. When endodontic treatment is not effective, endodontic surgery may be able to save the tooth.